Overview Diabetic Retinopathy | Treatment Options | Assistive Technology
Overview of Diabetic Retinopathy
Diabetic retinopathy is an eye condition that can affect people with diabetes; it is also a leading cause of blindness in adults. Specifically, diabetic retinopathy damages the part of the eye known as the retina, which plays an essential role in vision. Treatment for diabetic retinopathy depends largely on the extent of damage done to the retina by the disease.

Diabetes is a condition characterized by high levels of blood sugar, also known as glucose. The cells of the body use glucose as energy. When healthy people eat, their digestive tract absorbs glucose and sends the sugar into the bloodstream. As their cells absorb and use the glucose, their blood sugar levels go down. In people with diabetes, though, the cells have a hard time absorbing sugar from the bloodstream, so their blood glucose levels stay high all of the time; doctors refer to this as hyperglycemia. Excess sugar in the bloodstream can damage body tissue, especially those tissues that contain large numbers of blood vessels.
eSight electronic eyewear enhances vision for people living with vision loss, blurry vision, blind spots and more. Try eSight today!
The Retina
The retina of the eye is one such tissue – it contains many tiny blood vessels that deliver oxygen and nutrients to the cells of the retina, and that carry away blood and waste products from the retina. The retina requires a constant supply of blood to function properly.
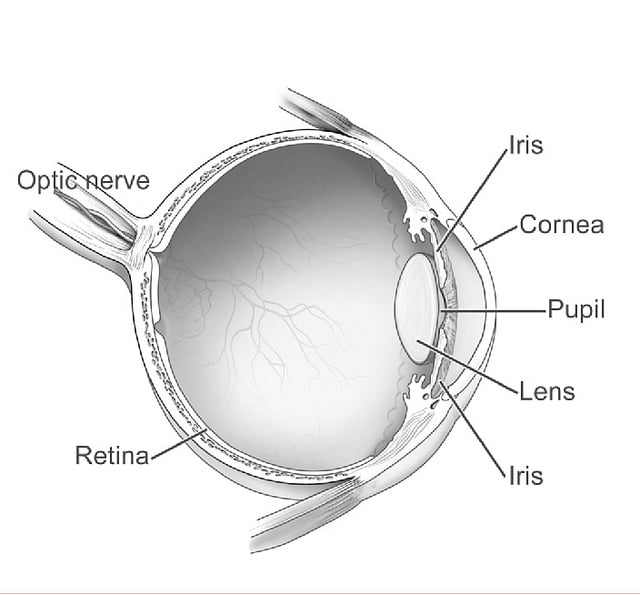
It also relies on vitreous humor, also known as vitreous gel, which is a transparent watery substance inside the eye. Vitreous humor provides nutrients, maintains the shape of the eye, helps absorb shock, and keeps the retina properly connected to the back wall of the eye.
Hyperglycemia
Chronic high blood glucose levels associated with diabetes can affect the blood vessels of the eye and, in some cases, affect the vitreous humor inside the eye. Specifically, hyperglycemia can damage the blood vessels near the retina, causing the blood vessels to leak blood and other fluids into the retina. The excess blood and fluid can cause the center of the retina, known as the macula, to swell and disturb vision.
The eye tries to improve blood circulation by creating new blood vessels on the surface of the retina. These blood vessels are often fragile and abnormal, and often leak fluid into the eye to block vision. The abnormal blood vessels can also grow into the vitreous humor and leak fluids, thereby clouding the normally clear liquid. Treatment would involve destroying the abnormal blood vessels and replacing the clouded vitreous gel.
The abnormal blood vessels can trigger the development of scar tissue, which can pull the retina away from the rest of the eye, a condition known as retinal detachment. Pulling the retina away from the rest of the eye can cause “floaters” and flashes of light that can interfere with vision. Abnormal growth of blood vessels, leaking fluids, scar tissue and retinal detachment can cause significant vision loss.

Two Types of Diabetic Retinopathy
Eye doctors classify diabetic retinopathy into two types:
Non-proliferative diabetic retinopathy (NPDR) – an early stage of diabetic retinopathy in which the blood vessels are weakened and may have bulges; fluid may leak from the blood vessels into the retina and cause the macula to swell
Proliferative diabetic retinopathy (PDR) – an advanced form of diabetic retinopathy in which circulation problems associated with diabetes prevent the retina from getting the oxygen it needs to function. The eye responds to oxygen deprivation by growing fragile, abnormal blood vessels in the retina; these blood vessels can even grow into the vitreous humor to cause vision problems.
Treatment often depends on the type of diabetic retinopathy and its severity.
Clinically-validated, eSight enhanced vision glasses are used by many people living with diabetic retinopathy. Try eSight today!
Diabetic Retinopathy Treatment Options
Patients with diabetes have limited options when it comes to treatment for diabetic retinopathy. Those with mild diabetic retinopathy may be able to control the disease by keeping blood glucose at normal levels. People with advanced diabetic retinopathy may require surgery or medications.
Vitrectomy as a Diabetic Retinopathy Treatment
Vitrectomy is a treatment for proliferative diabetic retinopathy, excessive eye floaters, and retinal detachment. It involves removing vitreous gel contaminated with fluids from damaged blood vessels. Removing vitreous gel during vitrectomy can also decrease pressure within the eye just enough to release tension on a detached retina, allowing the retina to return to its proper position at the back of the eye. In some cases, eye surgeons perform vitrectomy to provide better access to the retina so that they can perform a number of repairs, such as removing scar tissue, do laser repair of retinal detachments, or even repair holes in the macula.
During a vitrectomy, the ophthalmologist will make a small incision in the white of the eye (sclera). The eye doctor will use a microscope and small tools to remove the cloudy vitreous gel or scar tissue, or return the retina to its correct position within the eye.
Laser Surgery as a Diabetic Retinopathy Treatment
Laser surgery, also known as laser photocoagulation, shrinks blood vessels and stops them from leaking. It is not painful, although patients may feel a stinging sensation or see flashes of light during the treatment when the ophthalmologist applies the laser to their eyes. There are two main approaches to laser surgery for diabetic retinopathy:

Focal photocoagulation – seals specific leaking blood vessels in a small area of the retina, usually near the macula; the ophthalmologist targets and seals off specific blood vessels with a limited number of laser burns
Scatter (pan-retinal) photocoagulation – slows the growth of new abnormal blood vessels developing over a wider area of the retina. During a single treatment, the eye doctor may make hundreds of laser burns over the retina; the patient may need to undergo two or more treatment sessions
Surgery as a Diabetic Retinopathy Treatment
Ophthalmologists can perform eye surgery to remove blood or scar tissue from the eye if laser treatment is not possible because the damage to the retina is too advanced. Surgery can slow the progression of diabetic retinopathy – or even stop it in some cases – but it is not a cure. Because diabetes is a lifelong condition, future damage to the retina and vision loss is still possible.
eSight’s low vision electronic eyewear significantly enhances vision empowering you to explore new possibilities in school, work and home. See what’s possible with eSight.
Anti-VEGF Injections as a Diabetic Retinopathy Treatment
Diabetic retinopathy treatment may include injections of a medication, known as anti–vascular endothelial growth factor therapy (anti-VEGF), directly into the eye. The chemicals in the anti-VEGF prevent the formation of new blood vessels at the back of the eyes. Anti-VEGF injections can stop eye problems from getting worse and may even lead to an improvement in vision.

Doctors may recommend anti-VEGF injections as a standalone treatment or in combination with Patients typically undergo monthly injections at the beginning of treatment, and then undergo treatments less often as their diabetic retinopathy stabilizes. Local anesthetic administered prior to the injections to reduce discomfort.
Steroid injections as a Diabetic Retinopathy Treatment
An ophthalmologist will sometimes suggest injections of steroid medication instead of anti-VEGF into the eye, particularly if anti-VEGF injections do not help a particular patient.
Assistive Technology Alternatives to Medical Treatments
While these therapies can help treat some of the complications of diabetic retinopathy, such as the growth of abnormal blood vessels and cloudy vitreous gel, advanced sight-enhancing technology can significantly enhance vision for diabetics who have vision loss. For those with diabetic retinopathy who may be going through vision loss, eSight is an option.
eSight is a low vision eyewear device that stimulates synaptic activity from the remaining photoreceptor function of its users’ eyes. Many successful eSight users live with central vision loss commonly caused by diabetic retinopathy. DR can damage the blood vessels and tissues in the back of the eye, which can prevent the photoreceptors and retina from working well which often results in cloudy or blurred vision.

Fortunately, eSight can stimulate synaptic activity from the remaining photoreceptor function of the user’s eyes. As a result, eSight makes clearer vision possible, resulting in enhanced vision of up to 7 lines on a doctor’s eye chart. It uses a cutting edge camera, smart algorithms and high resolution screens. It provides the flexibility to read books up close with the same ease as seeing a crosswalk sign from a distance.
eSight eyewear is clinically proven to significantly enhance vision for people living with visual impairments and legal blindness. Discover if eSight is right for you!
